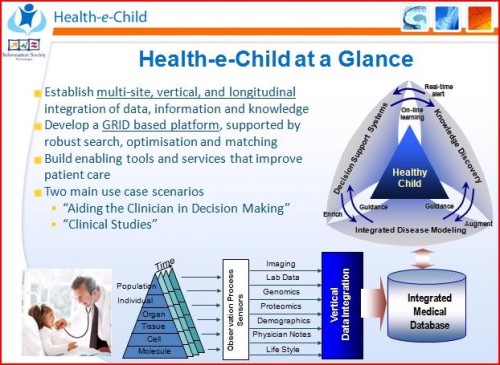
The Health-e-Child (HeC) project started in 2006 with the aim of developing a healthcare platform for European paediatrics, integrating traditional and emerging sources of biomedical information, from cell to tissue, organ, individual and population data. The focus areas of the project were congenital heart disease, arthritis and brain tumours in children. It addresses the critical need to integrate, exploit and disseminate knowledge from leading paediatric centres through advanced IT tools that facilitate the searching and matching of complex clinical cases and thereby to improve outcomes by personalising diagnosis and therapy in paediatrics.
Health-e-Child
Main achievements:
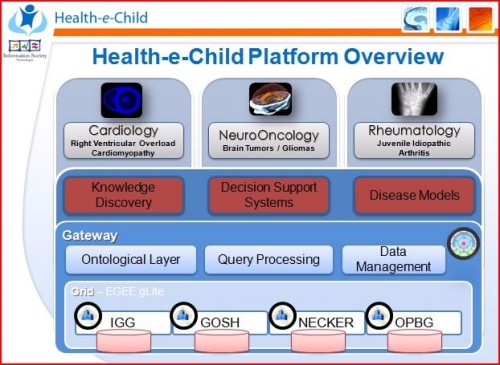
HeC goes beyond the traditional dependence on single-level or single-modality data and derives its analytical power from vertically integrated biomedical information from an unprecedented variety of sources. This new paradigm has been applied to all the three paediatric domains that were studied: cardiology, rheumatology and neuro-oncology. It opens up an entirely new and broad support for medical practice and research, especially with respect to children.
The project highlights and demonstrates the importance of large, heterogeneous repositories of clinically relevant data. Intervention and surgery planning benefit greatly from accessing and matching against previous cases.
HeC has pioneered the development of dynamic models of fast moving cardiac valvular apparatus with unprecedented morphological and temporal resolution. Such models, combined with existing models of the electromechanical physiology of the heart, contribute to better disease understanding and therapy planning, by providing a systemic view of the whole heart as a complex and long lasting pump.
The project has taken a major step towards the personalised management of juvenile idiopathic arthritis, by proposing the first MRI protocols to evaluate the progression of the disease, thus opening the potential for personalised treatment.
In addition, the project is furthering our understanding of childhood gliomas by developing a low cost chip that facilitates the analysis of 136 different mutations relevant to the formation and anamnesis of paediatric brain cancer. Many of these mutations are known to be related to the prognosis of the disease and predicting the response to treatment.
Taken together, these developments will directly contribute to European industry gaining a competitive advantage in both medicine and information technology.
The availability of HeC databases will enable researchers to conduct a new generation of epidemiological studies, based on much broader, better-integrated, and ’cleaner’ information. To reflect the results derived from such studies, European or national policies on medical issues may be modified thereby benefiting the lives of all citizens concerned.
The HeC platform has undergone a security assessment and has been in operation since 2008. It is currently securely and anonymously hosting the health records of patients enrolled for the project. Clinicians and researchers have since been making good use of its rich functionalities.
Socio-Economic Impact:
Infant and childhood diseases are a large and under-appreciated public health problem. Given that these patients have long lives ahead of them, the burden and costs are substantial for both families and society. HeC sheds new light on paediatric disease management.
Availability of the HeC databases and infrastructure can improve the success rates of resolving difficult medical cases and save children’s lives. Moreover, such improved medical decision-making can result in lower medical costs and treatment duration. New developments in both medical research and information technology become usable fostering personalised medical care, medical education, and medical information dissemination.
A Brief Case Study:
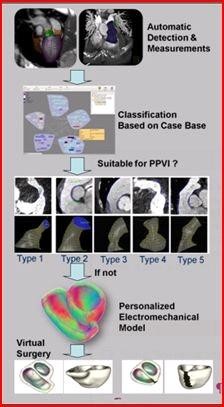
Tetralogy of Fallot is the most common cause of blue baby syndrome, a serious congenital heart disease requiring corrective surgery in infancy. As patients grow into their late teens and early adulthood they commonly suffer from severe pulmonary regurgitation. Clinicians facing the management of such conditions are confronted with complex treatment decisions, including pulmonary valve procedures in the majority of the cases.
The HeC project supports clinical decision making by improving disease characterisation and identifying similar cases across a network of leading hospitals:
A personalised model of the anatomy is extracted from advanced imaging to enhance diagnostic accuracy.
The patient’s heart is compared against a large repository of previously treated patients with known outcomes.
The morphology and dynamics of the pulmonary trunk help to determine whether a percutaneous pulmonary valve implantation (PPVI), a minimally invasive approach, can be attempted or whether surgical treatment is necessary.
In the latter case, a more sophisticated electromechanical model of the patient’s heart is used to virtually perform and evaluate the effects of the open-heart surgery.
More information about the Health-e-Child project can be found at the projects website (www.health-e-child.org) and on YouTube at www.youtube.com/HeCproject.